Who’s Responsible?

Notice
Although my case and this website focus on benzodiazepines, there is also a great deal of other psychotropic drugs (e.g. antidepressants, antipsychotics, opiates for pain etc) being mindlessly overprescribed to people from all walks of life including children, the elderly, disaster victims etc. which is seriously affecting all corners of society (See Effects on Us All).
In the video clip below Prof. Ashton explains that the medical profession should take much responsibility for allowing the situation (problems associated benzodiazepines and other prescribed psychotropic drugs) to arise.
She says they have been too easily persuaded by the drug industry and have been guilty of decades of thoughtless prescribing, muddled thinking, and blank acceptance of propaganda. She also sites that there has been a lack of training in clinical pharmacology and in the management of drug withdrawal.
She expresses concerns regarding an increase in off-label prescribing (indications for which the drugs have never been approved) which are affecting children (some as young as 2 years old) and the elderly in particular.
Sharing the same sentiments as Japan expert, Dr. Hirokuni Beppu who commented in my Japan Times article, Prof. Ashton also points out that doctors listening to patients has become a lost art. She adds that it was the patients themselves, and not the doctors, who first observed drug dependency with benzodiazepines and withdrawal symptoms from antidepressants.
Both Prof. Ashton and Dr. Hirokuni Beppu have expressed concerns over the influences of the pharmaceutical companies and government policies, and Prof. Ashton adds that doctors have also been seduced by the idea that drugs are the cure for mental illness when in fact they are not. She says it seems clear that today it is money, not science, driving pharmacology.
In closing, Prof. Ashton advises that “the public, that is all of us, should keep up the pressure on the authorities and should publicise what we see and hear every day from patients and health care workers.”
Top of Page
In the video clip below (from the 5:50 min mark) Prof. Ashton highlights some of the influences that pharmaceutical companies and government policies have on many of the addiction / dependency problems we see in our society today.
Prof. Heather Ashton
– History of Medicines Involuntary Addiction –
Vancouver, BC. April 4, 2006.
Quote from Dr Vernon Coleman, Life Without Tranquillisers, 1985.
"The biggest drug-addiction problem in the world doesn't involve heroin, cocaine or marijuana. In fact, it doesn't involve an illegal drug at all. The world's biggest drug-addiction problem is posed by a group of drugs, the benzodiazepines, which are widely prescribed by doctors and taken by countless millions of perfectly ordinary people around the world... Drug-addiction experts claim that getting people off the benzodiazepines is more difficult than getting addicts off heroin... For several years now pressure-groups have been fighting to help addicted individuals break free from their pharmacological chains. But the fight has been a forlorn one. As fast as one individual breaks free from one of the benzodiazepines another patient somewhere else becomes addicted. I believe that the main reason for this is that doctors are addicted to prescribing benzodiazepines just as much as patients are hooked on taking them. I don't think that the problem can ever be solved by gentle persuasion or by trying to wean patients off these drugs. I think that the only genuine long-term solution is to be aware of these drugs and to avoid them like the plague. The uses of the benzodiazepines are modest and relatively insignificant. We can do without them. I don't think that the benzodiazepine problem will be solved until patients around the world unite and make it clear that they are not prepared to accept prescriptions for these dangerous products."
(Source: benzo.org.uk)
Top of Page
In order to improve the situation several areas need to be addressed including: Preventative Measures / Education, Addressing Current Problem, Changing Attitudes, Post Withdrawal Rehabilitation / Compensation, Research.
Top of Page
The Bridge Project, Bradford
Annual Meeting, December 2011
INTRODUCTION
I am greatly honoured to be invited to speak to the Bridge Project. I admire all your aims and your progress to date. Of course, I am especially interested in your benzodiazepine withdrawal service, one of the few organisations which offers help to the million or more long-term prescribed benzodiazepine users in the UK. Thank you for giving me the chance to air some views on this subject.
HISTORY / BACKGROUND
Although today is a happy event, it is also a tragedy, 60 years after the introduction of benzodiazepines, that there is a need for a benzodiazepine withdrawal service. Why should we need charitable organisations with non-medical staff to help people having problems with drugs prescribed by their doctors? It is surely crazy. A long story has led to this situation to which doctors, drug companies, and government departments have all contributed interactively – a situation that has led to the suffering of many patients.
BENZODIAZEPINES
Benzodiazepines were introduced as a safer replacement for barbiturates which were causing a lot of problems, including drug dependence or addiction. That the dependence potential of benzodiazepines was overlooked by doctors casts shame on the medical profession which claims to be scientifically based. It was obvious that if one drug could replace another it must have common characteristics and usually a common mode of action. But the similarity between benzodiazepines and barbiturates was ignored.
In the 1970s there was a campaign called CURB in which doctors, egged on by the drug companies, were urged to prescribe benzodiazepines instead of barbiturates. They complied with such zeal that by 1978 Valium (diazepam) became the most commonly prescribed drug in the whole world. Many patients took it for years on end.
However, the benzodiazepines had never been tested for dependence or withdrawal effects. They were prescribed for anxiety, insomnia, and all the major and minor stresses of life such as going to the dentist, taking a driving test, taking an exam and much else. It was even suggested that Valium should be added, like fluoride, to the drinking water. Together people would be blessed both with tranquillity and strong teeth!
MARKETING
At about this time there was a change in the way drug companies were run. A pharmacologist working for Sanofi Pharmaceuticals remarked, “In the beginning the companies were run by chemists, but now most of them are run by people with MBAs, people who could be the chief executive of Renault or Volvo, for example. They don’t know about drugs” – But clearly, they do know where the market is.
The same pharmacologist reported, “When you find a drug that looks interesting, the problem comes when you present it to the company’s financial analyst. You say, I have an exciting new drug which looks medically useful. Good, says the financial analyst, what is the market? So you have to decide for what indication the drug should be developed. If the indication is not there, it must be created – in other words a disease suitable for the drug must be invented.”
One of the many examples of this process was the development of Xanax (alprazolam), a very potent benzodiazepine, for panic disorder. The marketing of this drug was designed to suggest that Xanax had unique properties that would displace diazepam (Valium) from the top market position. There was in fact nothing unique about Xanax, except its potency – (it was 20 times stronger than Valium). All the benzodiazepines, including Valium, could control panic attacks.
Xanax was duly marketed by Upjohn. It did control panics but at the cost of heavy sedation because 4-6mg doses were used – equivalent to 80-120mg diazepam. Nevertheless, Xanax overtook Valium as the most widely prescribed benzodiazepine. It was dropped by the NHS here because of adverse effects, but it is still widely prescribed in the U.S, Australia, Japan and other countries.
DSM CLASSIFICATIONS
Meanwhile, the physicians of the American Psychiatric Association, who produce the internationally accepted Diagnostic and Statistical Manual of Psychiatric Disorders (DSM), were working on a classification of anxiety disorders. In the new DSM III, panic disorder (the term invented by the makers of Xanax) became a separate anxiety state and anxiety was officially split into separate categories including panic disorder, agoraphobia, social phobia, generalised anxiety disorder and others. 60-100% of the panel members, who devised this classification, had financial ties to drug companies.
The inference of the new classification was that these separate disorders respond to different drugs. But in fact they all merge together – for example, if you have generalised anxiety you often get panic attacks; if you have panic attacks you are prone to agoraphobia etc. And all these categories respond to the same drugs including all the benzodiazepines. If they all respond to the same drugs and the symptoms are common to all types, they clearly cannot be separate entities. But they are still differentiated in the present DSM IV.
ADDICTIVENESS
The backlash came when the patients on long-term benzodiazepines themselves complained to their doctors that the drugs were addictive, mainly because they got withdrawal symptoms if they tried to stop. Eventually, in the early 1980s, controlled trials demonstrated beyond doubt that withdrawal symptoms from regular therapeutic doses of benzodiazepines were real, and often severe, and that they indicated physical dependence on the drugs. Finally, the medical profession accepted officially, on the grounds that they produced a withdrawal syndrome, that benzodiazepines were addictive if taken long term.
Z-DRUGS
Not to be outdone, the drug companies later produced the Z-drugs such as zopiclone and zolpidem. Although they are not benzodiazepines they act in the same way and also cause dependence and a withdrawal syndrome.
ANTI-DEPRESSANTS
With a declining popularity of benzodiazepines came a renewed interest in antidepressant drugs – especially as the Chief Medical Officer warned in 1980, that long-term benzodiazepines cause or aggravate depression and increase suicidal tendencies.
New antidepressant drugs were introduced in the shape of the SSRIs (selective serotonin reuptake inhibitors) in a deliberate tactic to displace benzodiazepines. Drug companies sponsored international symposia where speakers warned of the harm caused by benzodiazepines and suggested that SSRIs were not only good antidepressants but also worked for panic disorder, general anxiety, social phobia, post-traumatic stress and obsessive compulsive disorder.
And so in 1987 Prozac came on the scene and successfully ousted benzodiazepines as the most popular drug for depression, anxiety and general well-being.
But there is a sting in the tail of this story too. After a while it became apparent that SSRIs, like benzodiazepines, produced a similar withdrawal syndrome, when they were stopped. The doctors were surprised by this discovery and this was another example of their ignorance and lack of thought. It was already known that the older antidepressants produced a withdrawal reaction. Needless to say, the drug companies did not test SSRIs for withdrawal reactions.
DEFINITIONS
As previously mentioned, the benzodiazepines had been accepted as being addictive on the basis of their withdrawal effects. Now the all-powerful physicians of the American Psychiatric Association were faced with SSRI withdrawal. So once again they shifted their position. They adroitly changed their definition of drug dependence in the DSM IV. Withdrawal effects were no longer enough to qualify. The criteria for dependence were extended to include tolerance, dosage escalation and other characteristics. And the withdrawal syndrome was replaced by the patronising euphemism “discontinuation reaction”. As if a patient would think there was some subtle distinction between ‘discontinuation’ and ‘withdrawal’.
I can’t help thinking that there is something Orwellian in these manipulations, like the slogan in Animal Farm which started as “4 legs good; 2 legs bad”, but when pigs started walking on their hind legs the slogan was changed to “2 legs good; 4 legs bad”. In other words “discontinuation effects good; withdrawal effects bad”.
BIG PHARMA
So it seems that Big Pharma is slowly strangling the medical profession, like ivy growing up a tree, and forcing medical complicity with drug company aims – resulting in changed definitions of dependence and even new classes of mental illness.
Heads of drug companies earn enormous salaries. For example the head of Wyeth, which makes Ativan, is paid $24 million a year. There are as many Fat Cats in the drug industry as there are among bankers. The companies have used many methods to implement their drug sales. I can only mention a few.
One is to sponsor drug trials in which only the favourable results are published; negative results are suppressed. The company purchases thousands of reprints of their publications giving the journals a profit margin of 30%. Richard Smith, a former editor of the British Medical Journal, said, “An editor may face a stark conflict of interest: publish a trial that will bring in $100,000 of profit or fire a subeditor to meet your budget”.
A second method is to woo doctors by funding conferences at attractive resorts, with business class flight seats, large honoraria to speakers, free gifts and expensive dinners.
Thirdly, there are the drug reps who visit doctors in their offices. US drug firms employ around 100,000 drug reps at a cost of $5 billion a year. A successful rep campaign can bring in $10 for every $1 spent.
A fourth method is by advertising. The more heavily advertised a drug the greater the sales and the greater number of prescriptions, and the apparent incidence of the illness at which the drug is aimed to treat also increases.
ILLICIT DRUG SCENE
A combination of drug company promotions and doctors’ overprescribing has led to some tragic results, such as prescribed drugs entering the illicit drug scene. Nowadays most illicit drug abusers also take, and may inject, benzodiazepines – which can result in limb amputations, HIV infection and hepatitis C, among other complications. And BZs are now obtainable over the internet.
PROFITS vs. SCIENCE
It is clear that money, not science, is driving medicine. Of course the drug industry provides and promotes drugs with the aim of making money, while the medical profession prescribes these drugs with the aim of helping people.
Yet the drug companies are the only ones with enough money to develop new drugs which can, and have, saved many lives. At present there is a wave of medical opinion against the drug companies. But an unfortunate result has been to drive the two professions apart when they should be collaborating.
Partly because of increasingly strict regulations, there has been a decrease in the development of new drugs, thus denying some patients access to drugs that may help them.
Fortunately, there are some recent faint signs that the government is hoping to tackle this problem by earlier licencing of new drugs through the NHS and cooperative research between drug companies and Medical Research Council scientists. And drug companies are becoming slightly more transparent in their dealings.
THE PLOTICAL SYSTEMS
How is the government involved in this? Well, the Department of Health sponsors both the drug industry and public health matters. The same Department, indeed the same Minister, is responsible both for negotiating drug prices for the NHS (the NHS has to buy all our drugs) and for ensuring that NHS spending on drugs is sufficient to keep the UK drug industry profitable. In practice, the drug industry affects every level of health care provision from the licensing of new drugs, to the promotion of drugs to prescribers, and to the compilation of clinical guidelines.
In 2005 the House of Commons Health Committee issued a report on “The Influence of the Pharmaceutical Industry”. They recommended that the sponsorship of the drug industry should pass to the Department of Trade and Industry while the Department of Health should concentrate solely on public health.
This seemed a sensible recommendation but unfortunately the government rejected it. There is now an all party parliamentary group which aims to improve facilities for prescribed benzodiazepine users but so far with little effect. Meanwhile the government spends large amounts on drug abusers but virtually nothing on prescribed BZ users who do not ‘abuse’ drugs.
ACCOUNTABILITY
In a radio programme this year, Professor Lader, who was one of the first to document benzodiazepine problems, was asked why the Department of Health had not taken action, as the Department itself admits that there are over 1 million long-term, prescribed benzodiazepine users in the UK who receive little help in withdrawal.
His depressing reply was that the DOH is influenced by the powerful drug companies who would have to pay out millions of $/£ in compensation if the health risks of long-term benzodiazepines were exposed, and also that GPs are afraid of litigation from patients who have been prescribed long-term benzodiazepines. This is a corrupt state of affairs and, as always, it is the patients who pay the price.
WITHDRAWAL CLINIC
This takes me to the patients I saw in my withdrawal clinic. The clinic started as a clinical pharmacology unit at the Royal Victoria Infirmary in Newcastle for people who had adverse effects from any type of prescribed drugs. But in 1981 patients started to be referred because of adverse effects from benzodiazepines, and I was soon inundated with anxious patients wanting to come off their prescribed benzodiazepines which they had often been on for many years, 20 years or more.
They themselves had realised that the drugs, though initially effective, were no longer working and seemed to be actually making them feel ill. They had many symptoms such as anxiety, insomnia, depression and poor memory as well as physical symptoms. But if they tried to stop the drugs, the symptoms got worse and a host of withdrawal symptoms appeared. The effects of long-term benzodiazepines and withdrawal symptoms are shown in the handout. They are too numerous to mention here.
These patients felt that they were addicted and asked for help in withdrawal. I knew nothing at the time about addiction or withdrawal (which were not taught in medical school) but there were so many patients that I had to start a special benzodiazepine withdrawal clinic.
None of my colleagues wished to be involved, so I ran this clinic single-handedly for 12 years, from 1982-1994, when I had to retire from the NHS on grounds of age. Not knowing what else to do, I just listened to the patients and it was actually they themselves who taught me what I know about the effects of long-term benzodiazepines and about the effectiveness of slow tapered withdrawal.
I followed closely the progress of these patients week-by-week and sometimes day-by-day, and gradually, from their experiences, developed a generally applicable gradual withdrawal method. The success rate for these patients was nearly 90% and there were very few relapses.
SUPPORT
The experiences of these patients have been confirmed in many studies and by thousands of patients attending tranquilliser support groups in the UK, Europe and the US. Later, but too late, there were warnings from the DOH in 1980 and 1988 that benzodiazepines are indicated for short-term use only – ideally a maximum of 2-4 weeks.
Yet a recent GP study in Newcastle showed that there is still an average of 185 long-term (over 6 months) prescribed benzodiazepine users in every GP practice and probably over a million in the UK. No-one took over my clinic when I retired, and Professor Lader’s clinic in London also closed. So it is now up to organisations such as this one to provide services for these patients.
That is why I was delighted to hear about the Bradford benzodiazepine withdrawal service and the wonderful progress it has made since it started in 2008. The results have been summarised in an excellent report by Dr. Bray. I think the service has adopted exactly the right approach, which is for a specialist worker to cooperate closely with GPs and to operate within the GPs surgeries.
An experienced worker can give needed time, support and encouragement to patients while also educating the GPs about devising withdrawal schedules and the rational prescribing of benzodiazepines in general. At present I understand there is only one lone worker (Debbie Fielding who is a trained counsellor and drug worker). I hope it will be possible to extend the service to engage many more workers here in Bradford and that other organisations, all over the country, will follow your example.
LISTENING
Only those who give time to listen have any idea of the problems of individuals who, through failure of the present health system, and through no fault of their own, are driven to seek advice from organisations like the Bradford Service for practical help with benzodiazepine withdrawal.
Top of Page
WARNING
- Any information given on this site should not be substituted for the advice of a physician who is well-informed about benzodiazepine addiction and withdrawal.
- All information given here is therefore to be followed at your own risk (See Disclaimer).
- Abrupt cessation of benzodiazepines may be very dangerous. Always consult your prescriber if you are considering making any changes.
The primary language of this website is English. Japanese appears as translations only (except for some original court documents).
These translations have been done by many different translators including me. Therefore, there are differences in quality and styles.
Please understand that I am not native Japanese and subsequently there are parts that may sound unnatural in Japanese.
Cause for Alarm!

Consider this extract from:
A Review of David Healy's “The Psycho-pharmacologists III” by Professor Heather Ashton
How is it that the pharmaceutical industry has come to dominate the field?
Healy points out that drug companies “are now not simply confined to finding drugs for diseases. They have the power to all but find diseases to suit the drugs they have”.
Pierre Simon (Sanofi Pharmaceuticals) remarks: “In the beginning the pharmaceutical industry was run by chemists.
This was not so bad... Now most of them are run by people with MBAs... people who could be the chief executive of Renault, Volvo or anything.
They don't know anything about drugs.” The problem comes when a chemist presents an interesting drug to the financial analyst, who asks: “What is the market?”
The chemist has to decide for what indication the drug will be developed. If the indication is not there, it must be created.
It was difficult to get any relief from the ongoing symptoms

Unlike injuries where you may get some relief from adjusting your posture etc, with drug dependency in my case, the pain was both mental and physical and ran 24/7 regardless…
THE WRITING IS
ON THE WALL
for benzodiazepine use
Dr Andrew Byrne
Redfern NSW Australia
Benzodiazepine Dependence, 1997
“If any drug over time is going to just rob you of your identity [leading to] long, long term disaster, it has to be benzodiazepines.”
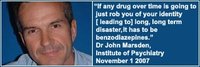
Dr John Marsden,
Institute of Psychiatry, London
November 1, 2007
“Benzos are responsible for more pain, unhappiness and damage than anything else in our society.”
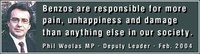
Phil Woolas MP,
Deputy Leader of the House of Commons,
Oldham Chronicle, February 12, 2004
“The benzodiazepines are probably the most addictive drugs ever created and the vast army of enthusiastic doctors who prescribed these drugs by the tonne have created the world's largest drug addiction problem.”
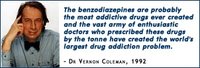
The Drugs Myth, 1992
“If there's a pill, then pharmaceutical companies will find a disease for it.”
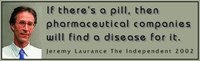
Jeremy Laurance,
The Independent, April 17, 2002.
“To rely on the drug companies for unbiased evaluations of their products makes about as much sense as relying on beer companies to teach us about alcoholism.”
Marcia Angell MD
(Former) Executive Editor New England Journal of Medicine
“It is more difficult to withdraw people from benzodiazepines than it is from heroin.”
Professor Malcolm H Lader
Institute of Psychiatry London
BBC Radio 4, Face The Facts
March 16, 1999
“Withdrawal symptoms can last months or years in 15% of long-term users. In some people, chronic use has resulted in long-term, possibly permanent disability.”
Professor C Heather Ashton
DM, FRCP,
Good Housekeeping, 2003
“Clearly, the aim of all involved in this sorry affair is the provision of justice for the victims of tranquillisers.”