Section Three
3. General
3.1 Recovery
3.1.1
Wayne’s recovery was made apparent by the following:
- Recovery from symptoms
- Ability to return to work
- Ability to return to recreational activities
- Ability to return to Japan
(1) Recovery from Symptoms
3.1.2
As outlined on page 12 of my first report, Wayne recovered from most of his symptoms within the first year of cessation with many symptoms subsiding within the first 3 months.
NB: Wayne did continue to suffer from panic attacks, however, this needs to be analyzed taking into consideration the long term effects including; protracted withdrawal, the trauma of the dependence experience, and the additional pressures of his subsequent case for compensation.
(2) Ability to Return to Work
3.1.3
Dr. Whitwell declared Wayne fit enough to return to work in June 2002 (See Evidence Koh A7). After being declared fit enough to return to work, Wayne worked as an English teacher for Queen’s Academy of English for 1 year (See Evidence Koh C5-2).
3.1.4
After ending the above employment contract, Wayne began working as a yardman for Placemakers for 1 year. This job involved handling bulk building supplies such as timber, cement, bricks etc (See Evidence Koh C5-4).
3.1.5
Wayne also worked as an adventure tour guide for Auckland Adventures. This job involved full day hiking tours, canoeing, snorkeling, horse riding, mountain biking, prolonged hours of driving etc (See Evidence Koh C5-7-2~21).
NB: Although, Wayne was able to make a return to employment, I understand he has been limited in his capacity to take on jobs that involve too much responsibility due to the panic attacks mentioned above, which was outlined in Psychologist, Alan Guy’s letter, dated 27th April 2007 (See Evidence Koh A18).
(3) Ability to Return to Recreational Activities
3.1.6
Wayne’s ability to return to recreational activities was made apparent in Article 3.1.5 above.
3.1.7
Following the reluctance of a local gym to allow Wayne a membership in 2001 (after he entered their training facility in an apparent state of poor health) Wayne began a physical training program, which over time resulted in significant gains in weight, strength and stamina. This is supported by the fact that he was able to maintain his capacity to work as an adventure tour guide and yardman outlined above.
(4) Ability to Return to Japan
3.1.8
Wayne’s recovery was made further apparent by his capacity to return to Japan, which was quite a psychological barrier for him following his previous experience there, as outlined in Psychologist, Alan Guy’s letter, dated 27th April 2007 (See Evidence Koh A18).
3.1.9
In summary of the above, Wayne’s condition upon presentation to our service was such that he was unable to work and was suffering from a range of physical and mental symptoms with obvious weight loss and loss in strength. In comparison, following the completion of his reduction program at our service, he was able to make a return to both work and recreational activities. Further, he was able to return to Japan once again to live and work, and despite being under much greater stress there now with his current claim for compensation, I understand that he continues to maintain a much better state of health at this present time.
Top of Page
3.2 Shortfalls in Prescription Doses
3.2.1
I understand that there have been some discrepancies regarding the apparent shortfalls in prescription doses. Also, I have been informed that a decision was made suggesting that because of these shortfalls (particularly in November 2000, when there was a shortfall of about 15 doses/5days worth) Wayne must have had the ability to miss consecutive doses, and therefore, could not have been in a state of dependence.
3.2.2
However, in accordance with our diagnosis, the overall clinical picture, and the application of the DSM-IV-TR, we know that Wayne was defiantly dependent.
3.2.3
In order to help clarify the potential for Wayne to have made it through the term of his treatment, despite being in a state of dependence, Wayne and his lawyer prepared an entire breakdown of every single dose administered to him under Dr. X and Dr. M during 2000 and 2001, which I have had the opportunity to view. Also, upon further consultation with Wayne, we were able to identify the following possibilities regarding the shortfalls.
- The possibility that Wayne commenced his prescriptions incrementally.
- The possibility that there were dosage surpluses from previous prescriptions, as there was in August 2000 (6 doses).
- The possibility that a dosage surplus was accrued during the early stages, due to forgotten doses, which is not uncommon in cases of long term treatment (however, Wayne’s ability to miss doses would have decreased with time as his dependency progressed).
- Left over doses from attempts at reduction, as Wayne reports was the case in November.
3.2.4
After considering the above, I can confirm that it would have been possible for Wayne to have made it through the duration of his treatment, despite there being apparent shortfalls, and despite the fact he was dependent, by way of accruing a reserve surplus.
3.2.5
Given that Wayne meet 5 out of the 7 criteria of the DSM-IV-TR, and given that it was possible for him to have made it through the treatment, despite there being apparent shortfalls in doses, this argument does not form grounds for ruling out dependence.
Top of Page
3.3 Differential Diagnosis (anxiety disorder)
3.3.1
I understand that Wayne was diagnosed with “Autonomic Nervous Disorder” by Dr. M at the O Medical Center, which I have been informed is a term commonly used in Japan to describe the suffering of psychosomatic symptoms caused by general life stresses / anxiety.
3.3.2
I also understand that there are two parts to the anxiety disorder argument, as follows:
- That Wayne was suffering from symptoms associated with stress.
- That Wayne was suffering from symptoms associated with a chronic anxiety disorder.
Before addressing each of these, I would like to clarify the terminologies below.
3.3.3
Generally, in English speaking countries, we do not use the term “Autonomic Nervous Disorder” to describe psychosomatic symptoms caused by general life stresses or anxiety conditions. It is more common to use the term “Anxiety”. As noted in “Management of Mental Disorders fourth edition” (Published by World Health Organization). “The experience of anxiety is very normal – moderate levels of anxiety will improve performance and even high levels of anxiety will be appropriate when they are consistent with the demands of the situation…. Individuals with anxiety disorders have specific and recurring fears that they recognize as being irrational or unrealistic and intrusive.”
3.3.4
Subsequently, in making this differential diagnosis, I have chosen to use the term “Anxiety Disorder” to include the range of disorders outlined in the DSM-IV and also defined by WHO. These include: Panic disorder, Agoraphobia, Social phobia, specific phobia, Generalised anxiety disorder, obsessive compulsive disorder, post traumatic stress disorder, acute stress disorder, anxiety disorder due to a general medical condition, anxiety disorder not otherwise specified, adjustment disorder, unexplained somatic complaints and hypochondriacal disorder.
3.3.5
In Wayne’s case I have excluded substance induced anxiety disorder because any anxiety symptoms Wayne potentially suffered from during the course of his treatment in 2000 ~ 2001 were likely to be secondary to the medication he was prescribed.
(1) Stress
3.3.6
Wayne has always made it clear that he had stress symptoms due to a stressful job in Shizuoka in late 1999 ~ early 2000, as outlined in Article 1.4.1 of my first report.
NB: I note these symptoms are also recorded on page 12 of the STRC Hospital ENT patient file and include fatigue / lethargy, pressure in temple areas, swelling of temporal veins, shortness of breath, although there was no mention of sweaty palms and racing / scattered thoughts.
3.3.7
Wayne reported to our service that most of these stress symptoms disappeared after changing jobs at the end of March 2000. However, there does not appear to be anything in the STRC Hospital ENT patient file to support this, although he did say on page 13 that he really liked his new job. He also said that he felt a bit tired from the first month’s training. In particular, he became a bit woozy around the middle of April. I am unable to comment as to whether this wooziness was related to the stress of his previous job or whether there was a separate cause.
3.3.8
Based on the above, we must also consider the possibility that Wayne did not recover completely from the aforementioned stress symptoms before commencing his treatment under Dr. X, as first believed.
3.3.9
In addition to the above stress related symptoms, Wayne has always made it clear that he had feelings of anxiousness over not being able to receive a clear diagnosis for his vertigo attack on 11th May 2000 and subsequent balance problem thereafter.
3.3.10
However, it must be made clear that even if Wayne still had the stress symptoms relating to his former job and anxiousness over not knowing what caused his vertigo attack, the presence of these symptoms do not detract from the fact that tolerance, withdrawal and dependency were formed for the reasons outlined in the DSM-IV-TR above.
(2) Chronic Anxiety Disorder
3.3.11
I have been informed that there have been claims made suggesting Wayne’s worsening of symptoms and development of new symptoms during the drug treatment was caused by a chronic inherent anxiety disorder, as opposed to dependency.
3.3.12
Below are indicators to suggest that Wayne did not have an inherent chronic anxiety disorder:
- No previous history of psychological or neurological complaints, as explained in Dr. ter Haar’s letter (Evidence Koh A19) and Dr. Alan Guy’s letter (Evidence Koh A18)
- No notable history of medical complaints whilst living in Japan for 3 years prior to 1999
- Initial testing and diagnoses in Japan did not indicate an anxiety disorder
- Anxiety disorder only diagnosed after Benzodiazepine exposure, as outlined in the O Medical Center patient file (Evidence Koh A6)
- First developed mental instability only after Benzodiazepine exposure - including panic attacks, anxiety, depression, mood swings, aggression, confusion, feelings of going mad
- There was no apparent increase in stressful events during the course of treatment (apart from the fact his condition was worsening and he did not know why)
- Was declared unfit to work only after Benzodiazepine exposure, as outlined in Dr. Whitwell’s letter (Evidence Koh A7)
- Condition improved following completion of initial withdrawal phase (See Article 3.1)
- Currently residing in Japan again and under more stress now with court proceedings, but maintaining better health
(3) Other Considerations
(Symptom Escape)
3.3.13
It could be argued that the ‘returning / worsening of symptoms’ during the treatment (Article 2.1.3) was due to symptom escape (where symptoms of the original complaint resurface). However, symptom escape also occurs as a result of tolerance and lost drug effect and therefore, this argument does not detract from the criteria of tolerance having been met.
(Illness Progression)
3.3.14
It could be argued that the ‘new symptoms’ during the treatment (Article 2.2.3) were due to illness progression. However, when put into context of the overall clinical picture, it becomes apparent that they were most likely due to withdrawal, as explained below:
- There was no apparent increase in stressful events during the course of treatment
- These new symptoms worsened again during the reduction program (symptom rebound) and then they all eventually eased off/disappeared once all Benzodiazepine prescribing was ceased.
- These new symptoms were accompanied by other new withdrawal symptoms during the reduction program, which also eventually eased off/disappeared once all Benzodiazepine prescribing was ceased.
NB: The exception to symptoms improving after the drugs were ceased was the panic attacks, which I understand have continued on and off to a lesser degree, whilst improving over time. With regards to the panic attacks, we must also take into consideration the long term effects including protracted withdrawal syndrome, the trauma of the dependence experience, and the additional pressures of the subsequent case for compensation.
(Dependency Can Produce Anxiety Symptoms)
3.3.15
Further to the above, we must also consider that dependency can produce the very symptoms they are designed to treat, i.e. anxiety symptoms, as noted by Professor Ashton based on a clinical study below.
“It is impossible to say whether the previously apparently stable patients would have developed psychiatric symptoms in the absence of benzodiazepine treatment. Nevertheless, the initial appearance of symptoms after a period of regular benzodiazepine use, the fact that all patients developed similar symptoms irrespective of the psychiatric history, and the improvement after drug withdrawal, all suggest that the symptoms resulted from benzodiazepine use and not from an underlying anxiety neurosis. This view has also been expressed by Lader, Tyrer, and others.
The appearance of symptoms while the patients were still taking benzodiazepines suggests the development of tolerance. Symptoms of prolonged use are said to include loss of concentration and memory, decline in psychomotor performance, depression, and emotional anaesthesia. With the exception of emotional anaesthesia, which was experienced only by the two patients with a history of depression, all patients developed these symptoms. Nevertheless, while the patients continued to take benzodiazepines they had other symptoms associated with benzodiazepine withdrawal - namely, agitation, panic attacks, agoraphobia, hallucinations, flushing, sweating, gastrointestinal disturbances, muscle pains, paraesthesiae, and many others. In several cases increased benzodiazepine dosage had been prescribed with temporary alleviation of the symptoms.” (See Benzodiazepine Withdrawal: An Unfinished Story. Prof. C. H. Ashton. 1984, Page 10/13 of online version).
(Pre-existing Symptoms)
3.3.16
It could be argued that many of Wayne’s symptoms were pre-existing and were therefore not related to dependency and withdrawal; however, it is not that simple. This is because in the case of dependency, pre-existing symptoms will often change in nature, frequency and duration, which can help us to differentiate between the original complaint and the development of withdrawal. Below are some examples in Wayne’s case.
3.3.17
Muscle stiffness – We know that Wayne already had muscle stiffness to begin, however, this changed in nature because, after it improved initially, it returned and worsened to the degree that his jaw began locking up, which is suggestive of withdrawal, as observed in a clinical study conducted by Professor Ashton below:
“Pain in various parts of the body was prominent. Neck pain and occipital headache, pain in the limbs described as aching, bursting, or cutting, and pain in the jaw were all common and often severe. Many patients complained of toothache, and some had undergone extractions of apparently normal teeth. Edentulous patients also complained of "toothache." All patients at some stage complained of a metallic or unpleasant taste. Stiffness and weakness often accompanied the neck, limb and jaw pains. Tremor of the hands and jaw, and muscle fasciculation, particularly in the thighs, were noted in several patients; many complained of sudden jerks, particularly in the legs but sometimes affecting the shoulders and back. Myoclonic jerks were observed in several patients.” (See Benzodiazepine Withdrawal: An Unfinished Story. Prof. C. H. Ashton. 1984, Page 8-9/13 of online version).
NB: According to Wayne’s medical records (Dr. ter Haar) Wayne had a previous history of periodic lower back pain since straining his back lifting heavy lumber in March 1989 and he also had a history of periodic neck pain, which according to Wayne, first developed in late 1997 whilst doing prolonged desk work using a laptop computer with poor ergonomics (Miyazaki Local Government Office).
However, the nature of Wayne’s muscle stiffness following 4~6 months of Benzodiazepine prescriptions was quite different in nature from the above, as Wayne began to experience jaw stiffness for the first time to the degree that he was unable to close his mouth properly. Further, Wayne reports that this muscle stiffness, which was previously limited to periodic episodes in the lower back and neck areas, came to encompass his entire body changing in nature from periodic to ongoing. Wayne reports that he subsequently developed the habit of massaging his thighs every evening at home.
This is supported by the fact that Wayne began a course of regular deep tissue massage from November 2000 at a local physiotherapy clinic in Saitama to help try and alleviate this. I have also had the opportunity to view an English transcript of the referral form from Dr. M to the above physiotherapy clinic in Saitama (T Physiotherapy Clinic), which says “has been suffering from increasing muscular tension in the upper rear region of his neck and shoulders”.
3.3.18
Hypersensitivity – We know that Wayne already had light sensitivity following his vertigo attack, however, this sensitivity changed in nature upon withdrawal because Wayne reports that he found the visual effects and volume of TV programs intolerable compared to other normal people around him. Further, this hypersensitivity came to include sensitivity to smell, which was apparent in that he sensed he was emanating an oily smell from his body odor. This type of hypersensitivity is suggestive of withdrawal, as observed in a clinical study conducted by Professor Ashton below:
“A characteristic feature of benzodiazepine withdrawal is a heightened sensitivity to all sensations - hearing, sight, touch, taste and smell. When extreme, these sensations can be disturbing. One lady had to stop all the clocks in the house because their ticking sounded unbearably loud; many have had to don dark glasses because ordinary light seemed dazzlingly bright. Some find that the skin and scalp becomes so sensitive that it feels as if insects are crawling over them. Heartbeats become audible and there may be a hissing or ringing sound in the ears (tinnitus). Many people complain of a metallic taste in the mouth and several notice strange, unpleasant, smells which seem to emanate from the body.” (See Benzodiazepines: How They Work and How to Withdrawal. Prof. C. H. Ashton. Revised August 2002 – Chapter 3, Pages 7/22 of online version).
(Differentiating Between Symptoms)
3.3.19
It has been asked how we can differentiate between symptoms of the original complaint and those of dependence. Admittedly, it can be very difficult to differentiate between these because, in some cases, the symptoms are very similar. This is why it is not possible to make any judgments simply based on analyzing a few symptoms. Rather, everything needs to be considered in context including the application of the DSM-IV-TR criteria.
3.3.20
Generally speaking, if the drugs are achieving the desired effect, the patient’s condition will no doubt improve. In cases of Benzodiazepine dependence, the patient will likely experience an initial settling of symptoms followed by symptom patterns consistent with tolerance (See Article 2.1). When this is then followed by a continual worsening of symptoms and the development of new symptoms during the treatment, it is suggestive of withdrawal symptoms; however, illness progression must also be considered (See 3.3.14). If the patient experiences an intensifying of these symptoms upon reduction (symptom rebound) together with the development of other new withdrawal symptoms, it is likely that the symptoms were due to dependence, as was in Wayne’s case.
3.3.21
Further, when these symptom patterns are put into context of the overall clinical picture (See pages 11~12, Report One) including prescription history, the inability to work following the treatment and then the ability to return to work following drug rehabilitation etc. and the application of the DSM-IV-TR (See Section Two above) including the unsuccessful attempts at reduction etc. it becomes clear that the worsening of symptoms and development of new symptoms during the course of treatment were most likely caused by dependence.
(Relevance of Anxiety Debate)
3.3.22
It must be made clear that the outcome of the debate regarding whether or not Wayne had an anxiety disorder does not alter the fact that he was Benzodiazepine dependent.
3.3.23
Anxiety disorders and Benzodiazepine dependence can and do coexist in some cases. Indeed many people who are prescribed Benzodiazepines do have an underlying anxiety related condition and this is sometimes why the drugs are prescribed to begin with. However, as previously mentioned, Benzodiazepines are highly addictive drugs and are only suitable for treatment lasting for no more than about two weeks because they in turn can cause anxiety.
3.3.24
To say that a patient was not dependent because they had an anxiety condition is unfounded and does not rule out the possibility of Benzodiazepine dependency. Anyone taking Benzodiazepines for any more than about 2 ~ 4 weeks is susceptible to developing tolerance and withdrawal, including people with anxiety disorders. Subsequently, the debate over whether or not Wayne had an anxiety disorder does not form grounds for ruling out these criteria.
Top of Page
3.4 Consistency of Previous Reports & Evidence
3.4.1
I understand there has been some concern expressed regarding the consistency of my previous reports in relation to the evidence (patient files). After having had the opportunity to view the patient files firsthand, I am able to confirm the following with regards to the symptoms history outlined in Section One my first report:
- Article 1.4.8 is consistent with the Patient Questionnaire Form on page 2 of the O Medical Centre patient file (Evidence Koh A6).
- Article 1.4.7 is consistent with Wayne’s handwritten note to Dr. X (Evidence Koh A26).
- Article 1.4.6 is consistent with Wayne’s handwritten note to Dr. X (Evidence Koh A12).
- Article 1.4.5 was based on Wayne’s reports that he experienced an initial settling of symptoms - this is supported by the initial improvement of his muscle stiffness outlined on page 8 of Dr. X’s patient file (Evidence Otsu A1).
- Article 1.4.4 is consistent with page 12 of Dr. X 's patient file (Evidence Otsu A1).
- Article 1.4.3 is consistent with a summarized version of page 11 of Dr. X 's patient file, where most of the symptoms are basically different words for the same thing, i.e. dizziness (Evidence Otsu A1).
- Article 1.4.2 was based on Wayne’s reports that most of his work related stress symptoms outlined in Article 1.4.1 mostly disappeared after he changed jobs in April 2000 (See Articles 3.3.6~3.3.10 for comments on this).
- Article 1.4.1 was based on Wayne’s reports that he was experiencing work related stress symptoms, which is consistent with pages 12~13 of the STRC Hospital ENT patient file (See Articles 3.3.6~3.3.10 for comments on this).
NB: These symptoms contained in Section One of my first report are also consistent with Wayne’s presentation to our service.
3.4.2
I note that there was some additional information contained in the patient files. However, none of this has any significant bearing on the application of the DSM-IV-TR Criteria or the dependence diagnosis.
3.4.3
In the Q & A document, between Mr. A and me, dated 19th December 2008, I suggested a number of possible mechanisms for most of Wayne’s symptoms outlined in sections 1.4.6 and 1.4.7 of my first report, and I also said that I was unable to comment further on some of Wayne’s symptoms. This is because further information was needed at the time in order to be able to make a more objective decision.
However, the fact that many of these symptoms intensified during the reduction process and the fact that they are consistent with known Benzodiazepines withdrawal symptoms, as well as other adverse effects, or Benzodiazepine symptom clusters, remains unchanged. Please note that these were listed as possibilities only, and as I mentioned in my second report, there are numerous clusters of symptoms / syndromes related to Benzodiazepine use including; tolerance, dependence, withdrawal, symptom escape, symptom rebound, side-effects etc, and it is usual for them to overlap somewhat.
Top of Page
3.5 Future Reports & Possible Testimony
3.5.1
I understand there are 3 main disputes regarding Wayne’s claim for compensation, as follows:
- Dependence
- Informed consent & monitoring
- Long term effects / damages
(Future Reports)
3.5.2
Regarding (2) above, I understand that the informed consent and monitoring part of Wayne’s claim was rejected at the initial hearing on the grounds that there was insufficient evidence / argument put forward with regards to this. Subsequently, I am happy to provide a report on informed consent and monitoring based on Wayne’s case in relation to the World Health Organization’s “Guide to Good Prescribing”.
3.5.3
Regarding (3) above, I understand that there is a dispute over long term effects with regards to Wayne’s post drug rehabilitation history. Subsequently, I am happy to provide a report on long term effects of Benzodiazepine use based on Wayne’s case.
(Possible Testimony)
3.5.4
With regards to my availability for a possible testimony, I am happy to travel to Japan for a court date. However, the actual time will have to be confirmed in advance with my employer, which will require several months notice in advance.
NB: On top of having submitted several reports regarding (1) above, it is preferable to submit reports regarding (2) and (3) above as well in advance of any potential hearing date. This will allow time to get all of the facts straight based on the evidence in order to help provide the most accurate information possible. By doing so, all parties will have the opportunity to view the reasoning in advance, and therefore, be able to prepare any questions that they may have, which I am happy to respond to.
Also, please understand that preparing these reports takes time, as I also have work commitments at the hospital and there is also the need to relay information between Wayne and his lawyer between two different languages.
Top of Page
The primary language of this website is English. Japanese appears as translations only (except for some original court documents).
These translations have been done by many different translators including me. Therefore, there are differences in quality and styles.
Please understand that I am not native Japanese and subsequently there are parts that may sound unnatural in Japanese.
THE WRITING IS
ON THE WALL
for benzodiazepine use
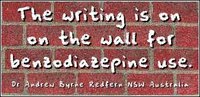
Dr Andrew Byrne
Redfern NSW Australia
Benzodiazepine Dependence, 1997
“If any drug over time is going to just rob you of your identity [leading to] long, long term disaster, it has to be benzodiazepines.”
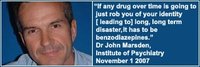
Dr John Marsden,
Institute of Psychiatry, London
November 1, 2007
“Benzos are responsible for more pain, unhappiness and damage than anything else in our society.”
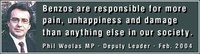
Phil Woolas MP,
Deputy Leader of the House of Commons,
Oldham Chronicle, February 12, 2004
“The benzodiazepines are probably the most addictive drugs ever created and the vast army of enthusiastic doctors who prescribed these drugs by the tonne have created the world's largest drug addiction problem.”
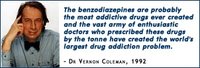
The Drugs Myth, 1992
“If there's a pill, then pharmaceutical companies will find a disease for it.”
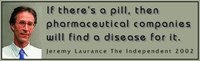
Jeremy Laurance,
The Independent, April 17, 2002.
“To rely on the drug companies for unbiased evaluations of their products makes about as much sense as relying on beer companies to teach us about alcoholism.”
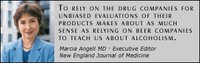
Marcia Angell MD
(Former) Executive Editor New England Journal of Medicine
“It is more difficult to withdraw people from benzodiazepines than it is from heroin.”
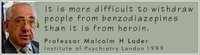
Professor Malcolm H Lader
Institute of Psychiatry London
BBC Radio 4, Face The Facts
March 16, 1999
“Withdrawal symptoms can last months or years in 15% of long-term users. In some people, chronic use has resulted in long-term, possibly permanent disability.”
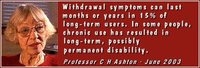
Professor C Heather Ashton
DM, FRCP,
Good Housekeeping, 2003
“Clearly, the aim of all involved in this sorry affair is the provision of justice for the victims of tranquillisers.”
The informed consent argument formed an integral part of the case because it was needed to prove negligence.

Without negligence there would have been no accountability, and therefore, no case from the outset.
In section 4 of his fourth report, Addictive Medicine Specialist, Dr. Graeme Judson explained the principles of prescribing and informed consent in relation to my case and sample applied.
The monitoring argument also formed an integral part of the case because it too was needed to prove negligence.

As above, without negligence there would have been no accountability, and therefore, no case from the outset.
As with informed consent, in section 4 of his fourth report, Addictive Medicine Specialist, Dr. Graeme Judson explained the principles of prescribing and monitoring in relation to my case and sample applied.
When do you suppose my condition was at its worst?
- When I was experiencing moderate levels of work related stress?
- When I was working a high pressure job and involved in a rigorous court battle in another country and language against a world famous doctor, the hospital, and the teams of lawyers and entire networks that no doubt sat behind them?
The answer is A.

Why?
Because at the time of situation (B) above, I wasn’t being mislead by a doctor feeding me a cocktail of highly addictive prescription drugs.
Instead I was employing the use of practical (non-drug) stress management techniques learnt in New Zealand before I returned to proceed with litigation in Japan.
Same principles applied to coping with the affects of the 3-11 disaster...
This section focuses on some of the apparent injustices of the Japanese courts in my case. To help highlight these, some parts of this section include cross-referencing between the High Court Verdict and the Dependency Reports which were all based on the official evidence and the DSM-IV-TR diagnostic criteria for dependency.
This section shows a variety of other benzodiazepine related videos that may be of interest.