Letter to Doctors

Dr. Jennifer Leigh
Dear Doctor,
It is understood that many doctors are not properly educated about Benzodiazepines. Please allow me to arm you with some basic facts so you can better help your patients, and avoid litigation that may be happening soon in the USA due to benzo prescribing.
I am Dr. Jennifer Leigh. I have a doctorate in psychology, post-doc Social Neurobiology studies, and I am an award-winning author. I was on a prescribed dose of Klonopin for 18 years for anxiety caused by traumatic life events.
I became ill on my steady dose and no doctor could tell me what was wrong with me. It took many months of research to discover that my health issues were caused by tolerance withdrawal to my prescribed dose of Klonopin.
Basic Facts:
Many people taking a prescribed dose eventually develop health problems.
Although Valium is considered the addictive drug, all benzos are equally addictive. Not in the way we think of addiction to street drugs, however, the dependency on the drug is very real. Remove the drug and withdrawal occurs.
The newer generation of drugs such as Xanax and Klonopin are more potent than Valium as they target sub-receptors on the GABA receptors. Scientists report that 1 milligram of Klonopin or Xanax is equal to 20 mgs of Valium.
Once exposed to the drug, the brain changes to accommodate the action on the chloride ring on the receptor. The theory is that eventually, the GABA receptor is absorbed into the neuronal axon, and is not available to do its normal function. This causes many benzo users who are on a steady dose to become anxious, as there are not enough working GABA receptors.
In this state, the body has more glutamate available than GABA. The HPA axis fires more often and the patient is less able to calm themselves. Anxiety and panic attacks are common side effects of long-term use of benzos, and is seen in patients who were prescribed the drug for medical reasons other than an anxiety or panic disorder.
Doctors who are not educated about the pharmacology of benzos diagnose this anxiety as a psychological problem instead of understanding it is tolerance withdrawal to the drug.
Patients who take a benzo on a daily basis, every other day, every few days, and even those who take it PRN can develop a long list of health problems that have been documented and verified by various health agencies and doctors. Some of the problems are: dizziness, headaches, anxiety, panic, gastrointestinal problems, depression, weakness, fatigue, lack of motivation, heart problems, temporary blindness, suicide ideation, tinnitus, depersonalization, bladder problems, IBS, etc.
Chemical dependency can happen in a very short time, the shortest on record is nine days. Dependency is not dose related. Patients on .25 of Klonopin have been recorded to have as equally severe withdrawal symptoms as those on higher doses.
When a patient wants to stop taking their benzo, it can become a life-challenging endeavor. (Long term use of benzos cause health issues, including dementia so no one should remain on a benzo for years.) Most doctors are unaware that benzos need to be tapered slowly, over a long period of time, in order to give the brain a chance to react to less of the drug, and to revert the use of the down-regulated receptors. Many doctors follow the rule of thumb for tapering opiates, however, this is far too quick and too big of cuts for benzo users. Additionally, it is difficult to taper from the more modern benzos, as they do not come in small enough doses. Xanax is especially difficult to taper as it is so short acting and inter-dose withdrawal can occur.
Even on a slow taper, many benzo patients become ill. Personally I became bedridden, unable to do the most basic of life’s tasks. I eventually was put in a detox ward, cold turkeyed with the help of Phenobarbital to avoid seizures, and sent home to recover on my own. This method is considered barbaric to most educated doctors, as it shocks the brain and can cause a protracted withdrawal. I was treated like an addict in the hospital and forced to participate in recovery activities when I could barely walk, or while hallucinating. Many benzo users are treated like addicts, even though we are chemically dependant, not drug seeking, and we are in that condition due to well meaning doctors who have prescribed the medication.
The recovery after taking the last dose can be a harrowing journey for many. We experience burning skin, deep bone and muscle pain, paresthesia, vision and hearing problems, gastro, heart, breathing, and balance issues, just to name a few. Because there are not enough working GABA receptors, we live in a world of terror and black depression, that makes our old psychological issues, (if there were any) look like child’s play. There are some reports that benzos also impact dopamine, serotonin, and other neurotransmitters, which may in part, explain the varied and intense problems brought about by withdrawal. (It has been shown that some catatonia patients are in benzo withdrawal, nothing more.)
Patients experiencing withdrawal are often misdiagnosed with schizophrenia, depression, and other psychiatric illnesses. They are often heavily medicated with antipsychotics, antidepressants, or placed back on their benzo. Some uneducated doctors prescribe Lyrica and Gabapentin for anxiety during withdrawal. These drugs work on the same receptors as benzos, and are not recommended. Alcohol, valerian root, and kava kava should be avoided as well for the same reasons.
Once the dose of a benzo has been lowered, it is often difficult to stabilize if placed back on the original dose. It is then harder to taper in the future. This little understood phenomenon is called “Kindling”. Although the action in the brain responsible for this is not understood, we are aware that it occurs.
Once off the drug, it can take a long time for the brain to recover from the damage done by a benzo; 6 to 18 months is the average time, however, many people, especially those who were on the drug for a long time, and those who were taken off cold-turkey, can have protracted withdrawal symptoms for years.
I am 25 months off of the drug, and still have burning in my spine, tingling, weakness, fatigue, bone and muscle pain, memory problems, cognitive issues, emotional issues (not my prior issues) and gastrointestinal problems. My withdrawal, like so many others, caused me to be unable to work or engage in life as I normally did. Many people in withdrawal face divorce, bankruptcy and loss of friends and social standing. A sizeable population in withdrawal are driven to suicide.
In summary, Benzodiazepines are dangerous medications as many people develop dependence and tolerance. Many develop illnesses, living with less than optimal health and their doctors are unsuspecting that it is the prescribed dose of a benzo causing their health problems. Getting off of a benzo can be life threatening. People can become very ill, unable to work, or socialize. This illness is often diagnosed as a return of the original anxiety and medicated with more benzos, antipsychotics, antidepressants, or other medications that are contraindicated for withdrawal. The only known cure from benzo withdrawal is the slow passage of time.
Here is a list of resources for you to educate yourself further. I thank you for taking the time to do so. Those of us who have been harmed by the prescribed use of benzos are hopeful that more doctors will be educated so they stop harming people by prescribing benzos for more than a few days. We hope too, that more doctors will learn how to correctly and successfully wean their patients off of benzos.
The only thing that I would like to add to the above is:
“The Committee on Safety of Medicines and the Royal College of Psychiatrists in the UK concluded in various statements (1988 and 1992) that benzodiazepines are unsuitable for long-term use and that they should in general be prescribed for periods of 2-4 weeks only.”
Non-drug options should always be considered first; weighing up potential risks against potential benefits.
Top of Page
THE WRITING IS
ON THE WALL
for benzodiazepine use
Dr Andrew Byrne
Redfern NSW Australia
Benzodiazepine Dependence, 1997
“If any drug over time is going to just rob you of your identity [leading to] long, long term disaster, it has to be benzodiazepines.”
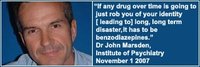
Dr John Marsden,
Institute of Psychiatry, London
November 1, 2007
“Benzos are responsible for more pain, unhappiness and damage than anything else in our society.”
Phil Woolas MP,
Deputy Leader of the House of Commons,
Oldham Chronicle, February 12, 2004
“The benzodiazepines are probably the most addictive drugs ever created and the vast army of enthusiastic doctors who prescribed these drugs by the tonne have created the world's largest drug addiction problem.”
The Drugs Myth, 1992
“If there's a pill, then pharmaceutical companies will find a disease for it.”
Jeremy Laurance,
The Independent, April 17, 2002.
“To rely on the drug companies for unbiased evaluations of their products makes about as much sense as relying on beer companies to teach us about alcoholism.”
Marcia Angell MD
(Former) Executive Editor New England Journal of Medicine
“It is more difficult to withdraw people from benzodiazepines than it is from heroin.”
Professor Malcolm H Lader
Institute of Psychiatry London
BBC Radio 4, Face The Facts
March 16, 1999
“Withdrawal symptoms can last months or years in 15% of long-term users. In some people, chronic use has resulted in long-term, possibly permanent disability.”
Professor C Heather Ashton
DM, FRCP,
Good Housekeeping, 2003
“Clearly, the aim of all involved in this sorry affair is the provision of justice for the victims of tranquillisers.”
This section focuses on some of the apparent injustices of the Japanese courts in my case. To help highlight these, some parts of this section include cross-referencing between the High Court Verdict and the Dependency Reports which were all based on the official evidence and the DSM-IV-TR diagnostic criteria for dependency.